Monday 14 July 2014
http://www.casereports.in/articles/4/2/Spindle-Cell-Sarcoma-Arising-from-Nerve-Sheath-Presenting-as-Huge-Abdominal-Mass.html
Spindle Cell Sarcoma Arising from Nerve Sheath Presenting as Huge Abdominal Mass
| Sohail Shaikh, Rajshree Dayanand Katke, Soham Dilip Raut
From the Department of Surgery1 and Department of Obstetrics & Gynecology2, Grant Government Medical College & Sir J. J. Group of Hospitals, Mumbai, Maharashtra, India.
|
||||||||
|
||||||||
|
||||||||
|
||||||||
Introduction
Spindle
cell sarcoma is a type of connective tissue cancer in which the cells
are spindle-shaped when examined on microscopy. The tumors generally
begin in nerve sheath, layers of connective tissue such as that under
the skin, between muscles, and surrounding organs, mesocolon, and will
generally start as a small lump with inflammation that grows. Spindle
cell tumors are low grade fibromyxoid soft tissue sarcoma and
microscopic appearance with features of both mesenchymal and
neuroendocrine differentiation. Cytogenetic studies of spindle cell
tumor show two cell lines containing balanced translocation between
chromosomes 7 and 16 [1].
A small group of both low grade fibromyxoid soft tissue sarcoma and
hyalinizing spindle tumor (HSCT) shows areas of increased cellularity
and atypia which are grouped as intermediate to high grade sarcoma [2]. A rare case of spindle cell carcinoma is documented in the esophagus [3]. These tumors rarely metastasize, but pulmonary metastases are documented [4,5].
Case Report
A
case of 65 year old female, housewife, presented through the outpatient
department with one month history of abdominal swelling and distention,
weight loss, intermittent constipation and dysuria. Her vitals were
within normal limits. On examination, abdomen was distended with everted
umbilicus, dilated veins on left lower quadrant of abdomen with a hard
non-tender mass almost occupying the whole of the abdomen arising from
pelvis reaching up to just 5 cm below xiphisternum with smooth surface.
Patient was previously operated for total abdominal hysterectomy with
bilateral salpingoophorectomy, seven years ago for ovarian cancer.
CT
scan report was suggestive of 19.5x16.3x13 cm well defined,
heterogeneously enhancing mass lesion with necrotic areas in the
midline arising from the pelvis and extending up to L3 vertebral body.
The mass was compressing the bladder though the fat planes were
maintained. The mass was reported most likely to be a neoplastic lesion
[Fig.1]. Midline exploratory laparotomy showed a jelly like mass in the
abdominal cavity and pelvis reaching up to the base of pelvis. The mass
was approximately 20x15 cm in size, smooth in surface and rounded in
shape [Fig.2]. Mass was separated from the surrounding structures and
excised. Weight of the mass was 4.5 kg, measured after the surgery.
Postoperative follow-up in the ward was uneventful and patient was
transfused for the compensating the blood loss of about 700 ml during
the surgery.
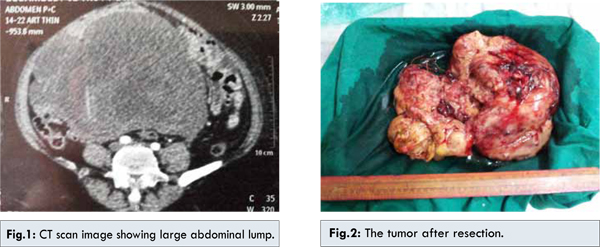
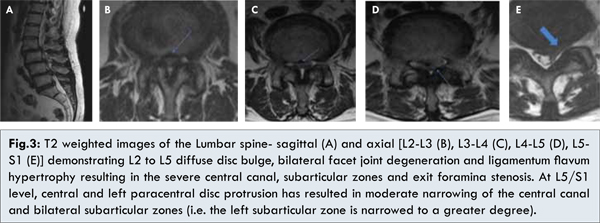
Histopathology
report was suggestive of high grade spindle cell sarcoma [Fig.3].
Several foci of tumor necrosis. nuclear pleomorphism and mitotic
activity were conspicuous. On immunohistochemistry, tumor cells were
positive for S-100 with negative Desmin and SMA. Thus possibility of
smooth cell differentiation was excluded and possibility of malignant
nerve sheath tumor favored. No ovarian parenchyma was recognized.
Patient was then referred to oncology for radiotherapy.
Discussion
Spindle
cell sarcoma is a type of connective tissue cancer in which the cells
are spindle-shaped when examined microscopically Spindle cell sarcoma is
a rare cause of large abdominal mass [6]. Cytological diagnosis of spindle cell tumor is difficult as compared to other soft tissue tumors [7].
These tumors generally begin in layers of connective tissue such as
that under the skin, between muscles, and surrounding organs, and will
generally start as a small lump that grows gradually. At first the lump
is self-contained as the tumor exists in earlier stages, and will not
necessarily expand beyond its encapsulated form. However, it may develop
malignant processes that can only be detected through microscopic
examination. As such, at this level the tumor is usually treated by
excision that includes wide margins through healthy-looking tissue,
followed by thorough biopsy and additional excision if necessary. In
high grade lesions, prognosis is grim and chemotherapy and radiation are
the only methods of controlling the cancer.
Spindle
cell sarcoma can develop for a variety of reasons, including genetic
predisposition but it also may be caused by a combination of other
factors including injury and inflammation in patients that are already
thought to be predisposed to such tumors. Spindle cells are a naturally
occurring part of the body’s response to injury. In response to an
injury, infection, or other immune response the connective tissues will
begin dividing to heal the affected area, and if the tissue is
predisposed to spindle cell cancer the high cellular turnover may result
in a few becoming cancerous and forming a tumor.
Spindle
cell tumors are usually diagnosed on histopathology based on picture
comprising of elongated spindle cells arranged in interlacing fascicles
and bundles with herring bone pattern at places. These bundles intersect
each other at wide angles at places showing storiform pattern with
eosinophilic cytoplasm and cigar shaped nuclei. Occasionally ghost cells
in the center and multinucleated giant cell may present, grading is
suggested in soft tissue sarcoma in order to improve the management,
prognosis and to prevent the recurrence, based on nuclear atypia,
nuclear overlap, mitotic figures, and necrosis these tumors are given
grades [8,9]. Treatment of spindle cell tumor is its complete excision [10].
Radiotherapy has minimal role and the tumor tends to recur. In our
case, spindle cell sarcoma of nerve sheath occurring in the abdomen was a
rare case. The size upto which it progressed posed a great challenge
during surgery as the tumor mass was jelly like and friable. The tumor
had to be meticulously dissected away from the small bowel at the same
time achieving adequate hemostasis.
References
| ||||||||
Wednesday 9 July 2014
International Journal of Reproduction, Contraception, Obstetrics and Gynecology
http://www.scopemed.org/?mno=35944
Regards
Dr Rajshree Katke.
M D (Obst & Gyanec), FIGOG
Medical Supertendent & Unit Head,
CAMA & ALBLESS Hospital, MUMBAI - 01
Regards
Dr Rajshree Katke.
M D (Obst & Gyanec), FIGOG
Medical Supertendent & Unit Head,
CAMA & ALBLESS Hospital, MUMBAI - 01
Caesarian deliveries more in private hospitals
Caesarian deliveries more in private hospitals
More caesarian deliveries are
carried out in private hospitals than public hospitals in the city, data of
last three years provided by BMC show. Last year, caesarian delivery rate in
private hospitals was 37.81%, while in civic hospitals it was 19.77 %.
Dr Rajshri Katke, medical superintendent, Cama and Albless Hospital, state-run maternity hospital at Fort, said: "A caesarian delivery should be undertaken only if there is a proven need for it. Here we encourage normal delivery unless there is some complications that will harm the mother or the child, or if the mother already has had C-section."
According to the health department data, the number of deliveries in civic-run hospitals and private hospitals are almost the same. However, the percentage of C-section remains higher in private hospitals.
Dr Niranjan Chavan, professor, gynaecology department, LTMG Sion hospital, one of the three tertiary care hospitals run by BMC, said: "In private hospitals, doctor-patient ratio is 1:1, and there is better care. Any complication is picked up fast. It has also been observed that doctors in private hospitals are very careful with their patients and don't want to take any risk."
Giving an example, Dr Chavan said in the case of a mild meconium-stained liquor, a fetal distress, a doctor in a public hospital would still take a chance, while in a private hospital, the doctor would opt for C-section.
"People going to private hospitals are very sensitive to pain, and the threshold of tolerance is less, and doctors don't want to take any chance," said Dr Chavan.
Agreeing with Dr Chavan, Dr Kiran Coelho, gynaecologist at Lilavati Hospital-Bandra, said: "Perinatal morbidity rate—affecting life of mother and child during pregnancy and/or the infant during first four weeks of life—is the valuation of obsetric cases which is always better in the private sector. Doctors in private sector are very careful and don't ignore even a small complication. There are many factors, like late marriages, increased infertility rate, etc that have contributed to the rise in C-section in private hospitals."
According to World Health Organisation guidelines, only 10-15% of births require surgical intervention in India. But many disagree with these guidelines as some gynaecologists believe several complications can arise during pregnancy which cannot be predetermined, and hence fixing a number would be difficult.
According to a study published in National Journal of Community Medicine, reasons that affect the rate of caesarean deliveries in India vary from psychological, the medical institution in question and socio-demographic factors. - See more at: http://mjn-e-news.com.my/june2014/special37.html#sthash.ayQzfKSk.dpuf
Dr Rajshri Katke, medical superintendent, Cama and Albless Hospital, state-run maternity hospital at Fort, said: "A caesarian delivery should be undertaken only if there is a proven need for it. Here we encourage normal delivery unless there is some complications that will harm the mother or the child, or if the mother already has had C-section."
According to the health department data, the number of deliveries in civic-run hospitals and private hospitals are almost the same. However, the percentage of C-section remains higher in private hospitals.
Dr Niranjan Chavan, professor, gynaecology department, LTMG Sion hospital, one of the three tertiary care hospitals run by BMC, said: "In private hospitals, doctor-patient ratio is 1:1, and there is better care. Any complication is picked up fast. It has also been observed that doctors in private hospitals are very careful with their patients and don't want to take any risk."
Giving an example, Dr Chavan said in the case of a mild meconium-stained liquor, a fetal distress, a doctor in a public hospital would still take a chance, while in a private hospital, the doctor would opt for C-section.
"People going to private hospitals are very sensitive to pain, and the threshold of tolerance is less, and doctors don't want to take any chance," said Dr Chavan.
Agreeing with Dr Chavan, Dr Kiran Coelho, gynaecologist at Lilavati Hospital-Bandra, said: "Perinatal morbidity rate—affecting life of mother and child during pregnancy and/or the infant during first four weeks of life—is the valuation of obsetric cases which is always better in the private sector. Doctors in private sector are very careful and don't ignore even a small complication. There are many factors, like late marriages, increased infertility rate, etc that have contributed to the rise in C-section in private hospitals."
According to World Health Organisation guidelines, only 10-15% of births require surgical intervention in India. But many disagree with these guidelines as some gynaecologists believe several complications can arise during pregnancy which cannot be predetermined, and hence fixing a number would be difficult.
According to a study published in National Journal of Community Medicine, reasons that affect the rate of caesarean deliveries in India vary from psychological, the medical institution in question and socio-demographic factors. - See more at: http://mjn-e-news.com.my/june2014/special37.html#sthash.ayQzfKSk.dpuf
Reference Link
The mother of all banks (http://afternoondc.in/)
The mother of all banks
Saturday, May 12, 2012

SHWETHA KANNAN reports
Tomorrow is Mother’s Day and the first connect between a new born baby and its mother is the time when she breastfeeds her child. While some mothers keep their children away from this privilege because of myths like colostrum, the first milk that is secreted after birth is not good, breastfeeding leads to the mother losing her figure etc., there are some mothers who are not able to provide their little ones with their milk because of poor health or other reasons. For such mothers, a milk bank is a ray of hope.
Jayashree Ramchandra (21) from Walkeshwar delivered a baby boy through caesarean on April 21, 2012. But it wasn’t an easy delivery because Jayahsree was hypertensive and the foetus was underweight. When her blood pressure shot up during the 30th week of gestation, doctors at the Cama and Albless Hospital at CST had to induce labour for the betterment of the mother and the unborn child. But when the induction failed and she couldn’t deliver vaginally, she had to undergo a caesarean. And this was how her 1.2 kg bundle of joy was born. Because of these complications, Jayashree faced some issues with regards to lactation and was worried about the nutrition of her child. But her worries were put to ease thanks to the fully functional human milk bank at the hospital. For eleven days, the baby was enriched with nutrition that a mother’s milk provides a baby with, as she was given the human milk stored at the hospital’s human milk bank. The child is now better and the mother full of smiles.
Another such mother is 28-year-old Noorjahan from Mazgaon, Mumbai. Her baby girl born on April 24, 2012 was a pre-term baby. After delivering the baby in the eight month of pregnancy, Noorjahan too had some issues with lactation, but because of the human milk bank at the Cama and Albless Hospital her baby is doing good and gaining weight.
Both Jayashree and Noorjahan feel that the concept of human milk banking is very useful and helpful as it provides the baby the essential nourishment when required the most. True. Why waste mother’s milk, which is no less than nectar for a child, by simply discarding it, when it can be used to give another baby the gift of good health?
This thought prompted Rajesh Bokadia, President, Rotary Club of Mumbai, Nariman Point (RCMNP) to start the initiative of establishing human milk banks in the city, making his club the first one to have started an initiative of this kind.
“Human milk banking is an issue that needs to be talked about especially in a country where thirty per cent of new born babies do not get the required quantity or quality of mothers’ milk. Mother’s milk is very essential for the baby’s growth and nutrition. While a lot is being talked about blood donation and other such causes, this issue addresses the need of the baby from the time it is born and hence is also equally important,” said Rajesh.
In this initiative, the RCMNP bears all the expenses of getting the equipments required for milk banking, sprucing up the place so that it looks like a milk bank etc. All they require from the hospitals is space to set up the bank. And Rajesh informed us that getting space and convincing the hospital authorities is the most difficult part.
“People have several reservations about milk banking and thanks to the bureaucracy and red tapism, getting a space to set up a milk bank at a hospital is difficult. We bear all the expenses of setting up the bank,” said Rajesh. Setting up a human blood bank requires around eight to ten lakhs. The hospital has to bear the recurring expenses which are negligible said Rajesh. The RCMNP has established two human milk banks in the city at J.J. Hospital, Cama and Albless Hospital and one at Dinanath Mangeshker Hospital at Pune and one at the Rajiv Gandhi hospital at Thane.
While this issue needs to be addressed with more vigour, the current set ups at JJ and the Cama and Albless Hospital, are doing well and the response from women to this initiative seems to be encouraging.
“The response to human milk banking is good but more needs to be done. The concept of human milk banking is extremely important and useful because babies who are under weight, are not able to suckle well or whose mothers aren’t able to lactate in sufficient quantities due to various reasons can benefit from such banks,” said Dr. Rajshri Katke, Medical Superintendent, Cama and Albless Hospital, where the human milk bank has been functional since 2007. The human milk bank at JJ too seems to be getting a good response. “Women, when properly informed, willingly donate milk. We collect nine to ten litres of milk per month,” said Dr. Ashok Rathod, head of the paediatric department, JJ Hospital.
So while the milk banks are doing their bit, what are the reasons not all women lactate in quantities that is enough to take care of the needs of her own child but also help other tiny tots get their share of good health? According to Dr. Suman Bijlani, Consultant Gynaecologist, Kohinoor Hospital and Director, Gyneguide clinic, the main reason for women not being able to breastfeed is lack of confidence.
“Fears like not being able to breastfeed the child or that the quantity wouldn’t be enough, affect lactation adversely. Then comes lack of education about lactation techniques like the correct way holding the baby, sitting in a position that will not tire the mother, giving the baby entire area and not only the nipples for suckling.
“Not knowing the correct latching techniques (the way the baby latches on the breast) which leads to cracked nipples and cracked nipples lead to painful breastfeeding, which might become a deterrent for breastfeeding,” concluded Dr. Bijlani.
Benefits of breastfeeding for the child and the mother
Breast feeding makes the child strong and gives it protection from infections. Mother’s milk provides up to thirty per cent of a child’s energy till the age of two. For mothers, breastfeeding provides protection against breast and ovarian cancers, osteoporosis and anaemia and helps facilitate the process of coming back to normal physical status.
What if a mother does not breastfeed?
Putting on excess weight; the necessary tissue changes that have to take place would not take place, which may lead to cancer. Toning of the abdominal tissues wouldn’t be proper and she may have to put in extra efforts, which, if she had breastfed her child, would have taken place naturally.
“During the first six months, the baby should be exclusively breast-fed and, after that, during the next six months, the baby can be given cow’s milk, mashed potatoes, moong water, etc., along with mother’s milk.”
Dr. Rajshri Katke, Medical Superintendent,
Cama and Albless Hospital
Reference Link
http://afternoondc.in/city-news/the-mother-of-all-banks/article_55375
Mumbai woman gives birth to baby weighing 4.5kg @ CAMA Hospital MUMBAI.
Mumbai woman gives birth to baby weighing 4.5kg
Nov 24, 2011, 10:45 IST | Agency: Mumbai | Place: #731643;#000;'>DNA Correspondent
A 28-year-old woman who arrived at the state-run Cama and Albless Hospital for Women and Child hospital in advanced labour, with the head of the baby jutting out of her, has delivered a boy weighing 4.5kg. The baby, who hasn’t been named yet,is 55 cm tall.
A team of three doctors used special manoeuvres during a three-hour procedure to deliver the baby. The mother, Anjali Sugur was brought to the hospital on Tuesday morning after she went into the labour and delivered at 10 am. This is her fourth child, and the delivery was normal.
India’s heaviest baby was a baby girl born in Surat last year. She weighed 5.7kg. The normal weight of an Indian newborn is between 2.5 and 3.5kg.
Dr Rajshri Katke, medical superintendent, Cama and Albess hospital said, “Though this is Anjali’s fourth delivery, this was her first delivery in hospital. The first three babies were delivered at home. She had registered herself soon after her pregnancy was detected and was regular in her check-ups.”
Last year, the hospital delivered a 4.3kg baby.
According to the doctors, she would have landed the baby and herself in trouble if she had not come to hospital for delivery. “It was good decision taken by the family as it requires skillful doctor to deliver such a huge baby. She would have risked her and the baby’s life otherwise,” said Dr Katke.
Doctors were surprised that such a huge baby was delivered by a non-diabetic mother. “Normally, overweight babies are delivered by diabetic mothers. In Anjali’s case, we knew that the baby is huge but since she was non-diabetic we got worried. We are happy that her delivery was normal,” said Dr Katke.
The baby is presently in under observation in the neonatal intensive care unit.
“Such overweight babies are prone to develop hyperglycaemic conditions in which the amount of blood glucose (sugar) in the blood is lower than normal. His sugar levels were low yesterday,” said Dr Katke.
The mother has been asked to breast-feed the baby frequently. “Such babies have to be fed more frequently than a normal newborn as the they need glucose more,” Dr Katke added.
Meanwhile, Anjali and her family can’t wait to take the new family member home. “I am very happy that my baby is so healthy. I am happy that I decided not to deliver the baby at home and came to hospital,” said Anjali.
Dr Sudeshna Ray, consultant of gynaecologist and obstetrician, Jaslok hospital and member of the committee of medical disorder in pregnancy said,“It is a challenge for both the mother and the obstetrician to deliver an overweight baby normally.”
“Overweight babies are born to the mother has diabetes mellitus during pregnancy, the mother has excessive weight gain during pregnancy or where the woman has delivered more than two babies before,” Dr Ray added.
Reference Link
http://www.west-bengal.com/health/mumbai-woman-gives-birth-to-baby-weighing-4-5kg/131488.html
Regards
Dr Rajshree Katke.
M D (Obst & Gyanec), FIGOG
Medical Supertendent & Unit Head,
CAMA & ALBLESS Hospital, MUMBAI - 01
Woman Conceives 8 Yrs After Tubectomy (http://www.aarogya.com)
Woman Conceives 8 Yrs After Tubectomy
Times of India02 July 2010
33–year–old’s pregnancy mistaken for stomach infection
A33–year–old woman who underwent tubectomy in 2002, has stumped the medical fraternity by conceiving again. Doctors were initially treating Yogita Waghela for a stomach infection leading to a swollen tummy, but later at Cama and Albless Hospital they stumbled upon the foetus growing inside her fallopian tube.
Waghela who was suffering from acute abdominal pain, consulted a general practitioner who allegedly treated her for stomach infection. She was also admitted at a local hospital for a few days, where she underwent a sonography twice but the doctors were unable to detect her pregnancy. It was only when she reached to Cama and Albless that doctors discovered her pregnancy.
"Waghela was brought to the hospital in a very critical condition. She was bleeding from her vagina, and her blood pressure was low," said Dr Rajshree Katke, associate professor of Obstetric and Gynaecology at the hospital. "We immediately shifted her to the ICU for an operation."
Dr Katke added that because of the late diagnosis, Waghela’s fallopian tubes had ruptured and she had already developed septicaemia. "We removed the 12–week foetus from her tube. She is out of danger now," she clarified, adding, "This is one of the rarest cases I have seen in my 20–yearcareer."
"Pregnancy after eight years of tubectomy is extremely rare. Nobody diagnosed her pregnancy because nobody thought that she could conceive. Her sonography report shows that there is a mass in her tube but no one thought that could be a foetus," said Dr Katke.
Waghela who is still in a shock, said, "I was getting my periods and was under the impression that the stomach ache was because of some infection. I had been popping pain killers for one whole month! I am thankful to the doctors who saved my life."
Yogita married Ramesh Waghila in 1999 and after bearing two children she went for a tubectomy in 2002. Her daughter is 10 years old while the son is seven years of age.
Disclaimer: The news story on this page is the
copyright of the cited publication. This has been reproduced here for
visitors to review, comment on and discuss. This is in keeping with the
principle of ‘Fair dealing’ or ‘Fair use’. Visitors may click on the
publication name, in the news story, to visit the original article as it
appears on the publication’s website.
Reference Link
http://www.aarogya.com/news-and-updates/year-2010/5930-woman-conceives-8-yrs-after-tubectomy-.html
Rarest of rare: Mumbai doctors Dr Rajshri Katke remove 20kg tumour from 50-yr-old (www.dnaindia.com)
Rarest of rare: Mumbai doctors remove 20kg tumour from 50-yr-old
The tumour originated from the woman's ovaries and was
attached to the abdominal wall, intestines and liver.
Doctors at Cama and Albless hospital in Fort where she was operated upon say they have never seen such a huge tumour and it is possibly the heaviest tumour successfully removed in the country. They now want to send the case study for publishing in a medical journal.
“When Shobha Kolhe met us in December, she was suffering from severe breathlessness. Her stomach was so bloated that she looked like a pregnant woman carrying four-five kids,” Dr Rajshri Katke, medical superintendent of Cama and who headed the operating team, said.
Many hospitals refused her admission as she was frail and considered a high risk patient. “I had recurrent fever and weakness since July. A local doctor gave me some medicines and I felt better,” Kolhe said. “But suddenly my stomach started bloating. We did not have the money to get a CT scan or sonography done.”
She was mentally harassed too, the woman said. Neighbours taunted her for being “pregnant at this age”. “They thought I was carrying... I used to cry in private. Also, I was afraid that I would die because all doctors told me that I had no chance of surviving.”
At Cama hospital, doctors took her up for surgery after the tumour showed up in a CT scan. The tumour originated from her ovaries and was attached to the abdominal wall, intestines, and liver. It pushed her diaphragm, making her breathless. “Never in my medical practice have I seen such a huge tumour. We were worried because she was so fragile,” Katke said. “The operation went on for 90 minutes. She was lucky that the tumour was not cancerous.” Kolhe will be discharged on Monday.
Experts say Kolhe had a mucinous cystadenocarcinoma of the ovary, a rare malignant form of ovarian mucinous tumours. This type accounts for 5-10% of all ovarian mucinous tumours.
“Giant benign ovarian tumours are a rarity nowadays because most cases are detected early during routine check-ups,” Katke said. “Ovarian cysts can turn malignant but fortunately most are benign.”
Dr Sudeshna Ray, consultant gynaecologist and obstetrician, Jaslok hospital, said: “Ovarian tumour has the tendency to grow faster and bigger... But 20kg is unheard of and unbelievable.”
Dr Ashwini Bhalerao Gandhi, consultant gynaecologist and obstetrician at PD Hinduja hospital, said: “We have seen several big tumours but not 20kg. This is certainly unheard of and happened because the family delayed taking medical help. She is lucky that the tumour was not cancerous.”
http://www.dnaindia.com/health/report-rarest-of-rare-mumbai-doctors-remove-20kg-tumour-from-50-yr-old-1948294
Tuesday 8 July 2014
United Nations Secretary-General Ban Ki-moon leads a high-level mission to India in support of the Every Woman Every Child initiative
Date: 04 May 2012
 Dr.Rajshree Katke Giving Presentation to United Nations Secretary-General Ban Ki-moon regarding the HIV Clinic.
Dr.Rajshree Katke Giving Presentation to United Nations Secretary-General Ban Ki-moon regarding the HIV Clinic.
The UN delegation visited Cama Hospital and the Sir J.J. Hospital—two leading health facilities in the Indian state of Maharashtra that provide health services for pregnant women and children.
On 28 April, United Nations Secretary-General Ban Ki-moon led a high-level mission to Mumbai, India in support of the Every Woman Every Child
initiative. During the visit, the Secretary-General commended Indian
officials for the progress made in the AIDS response. Mr Ban also
encouraged the Government of India to continue efforts to eliminate new
paediatric HIV infections by 2015—one of the objectives of the Secretary-General’s five-year action plan.
The Every Woman Every Child initiative is a global effort that was launched in 2010 by Secretary-General Ban Ki-moon to mobilize and intensify global action to save the lives of 16 million women and children and improve the lives of millions more.
Mr Ban was joined by senior UN health officials including the Director-General of the World Health Organization Margaret Chan, the Executive Director of the UN Population Fund Babatunde Osotimehin, the Executive Director of the Joint United Nations Programme on HIV/AIDS, Michel Sidibé, the Deputy Executive Director from the UN Children's Fund, Geeta Rao Gupta and the United Nations Secretary-General’s Special Envoy for Malaria Ray Chambers.
During the visit the Secretary-General, Mrs Ban and his delegation visited Cama Hospital and the Sir J.J. Hospital—two leading health facilities in the Indian state of Maharashtra that provide health services for pregnant women and children.
Mr Ban’s mission concluded with a high level reception hosted by Millennium Development Goals advocates Mukesh Ambani and Ray Chambers, which featured interaction with some of India’s leading AIDS activists, people living with HIV, business and government officials as well as film stars and sports legends. During the reception the Mr Ban announced the appointment of Mr Prasada Rao as his new Special Envoy for HIV/AIDS in the Asia-Pacific region.
 L to R: Millennium Development Goals advocate Mukesh Ambani, Kausalya
from Positive women network (PWN+), UNAIDS Executive Director Michel
Sidibé, Daksha Patel from Gujarat Network of People Living with HIV
(GNP+) and United Nations Secretary-General Ban Ki-moon.
L to R: Millennium Development Goals advocate Mukesh Ambani, Kausalya
from Positive women network (PWN+), UNAIDS Executive Director Michel
Sidibé, Daksha Patel from Gujarat Network of People Living with HIV
(GNP+) and United Nations Secretary-General Ban Ki-moon.
The UNAIDS Executive Director Michel Sidibé travelled to India’s capital New Delhi where he met with the Minister of Health and Family Welfare Shri Ghulam Nabi Azad. During their meeting, Mr Sidibé commended India for its new National AIDS Control Programme (NACP-IV) which was developed by national experts and will be funded primarily from domestic sources.
Mr Sidibé paid special attention to India’s role and contribution as a priority country in the implementation of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. It is expected that the national recommendations on the elimination of new HIV infections among children in India will phase-out of single dose nevirapine in the coming months. Mr Sidibé had the opportunity to see first-hand how services to prevent mother-to-child HIV transmission are being scaled-up at the Ambedkar Hospital, one of Delhi’s largest hospitals.
A high level round table organized by the Federation of Indian Chambers of Commerce and Industry (FICCI) and UNAIDS brought together more than 50 participants including leading representatives from the Indian pharmaceutical industry and the government under the theme “India’s partnership with Africa in pharmaceuticals”. Mr Sidibé encouraged the Indian pharmaceutical industry to seize the opportunities to scale up access to HIV treatment in Africa and engage as strategic partner for the development of pharmaceutical production in Africa.
Reference Link
http://www.unaids.org/en/resources/presscentre/featurestories/2012/may/20120504india/
Regards
Dr Rajshree D. Katke.
M D (Obst & Gyanec), FIGOG
Medical Supertendent & Unit Head,
CAMA & ALBLESS Hospital, MUMBAI - 01

The UN delegation visited Cama Hospital and the Sir J.J. Hospital—two leading health facilities in the Indian state of Maharashtra that provide health services for pregnant women and children.
The Every Woman Every Child initiative is a global effort that was launched in 2010 by Secretary-General Ban Ki-moon to mobilize and intensify global action to save the lives of 16 million women and children and improve the lives of millions more.
Mr Ban was joined by senior UN health officials including the Director-General of the World Health Organization Margaret Chan, the Executive Director of the UN Population Fund Babatunde Osotimehin, the Executive Director of the Joint United Nations Programme on HIV/AIDS, Michel Sidibé, the Deputy Executive Director from the UN Children's Fund, Geeta Rao Gupta and the United Nations Secretary-General’s Special Envoy for Malaria Ray Chambers.
During the visit the Secretary-General, Mrs Ban and his delegation visited Cama Hospital and the Sir J.J. Hospital—two leading health facilities in the Indian state of Maharashtra that provide health services for pregnant women and children.
Mr Ban’s mission concluded with a high level reception hosted by Millennium Development Goals advocates Mukesh Ambani and Ray Chambers, which featured interaction with some of India’s leading AIDS activists, people living with HIV, business and government officials as well as film stars and sports legends. During the reception the Mr Ban announced the appointment of Mr Prasada Rao as his new Special Envoy for HIV/AIDS in the Asia-Pacific region.

The UNAIDS Executive Director Michel Sidibé travelled to India’s capital New Delhi where he met with the Minister of Health and Family Welfare Shri Ghulam Nabi Azad. During their meeting, Mr Sidibé commended India for its new National AIDS Control Programme (NACP-IV) which was developed by national experts and will be funded primarily from domestic sources.
Mr Sidibé paid special attention to India’s role and contribution as a priority country in the implementation of the Global Plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive. It is expected that the national recommendations on the elimination of new HIV infections among children in India will phase-out of single dose nevirapine in the coming months. Mr Sidibé had the opportunity to see first-hand how services to prevent mother-to-child HIV transmission are being scaled-up at the Ambedkar Hospital, one of Delhi’s largest hospitals.
A high level round table organized by the Federation of Indian Chambers of Commerce and Industry (FICCI) and UNAIDS brought together more than 50 participants including leading representatives from the Indian pharmaceutical industry and the government under the theme “India’s partnership with Africa in pharmaceuticals”. Mr Sidibé encouraged the Indian pharmaceutical industry to seize the opportunities to scale up access to HIV treatment in Africa and engage as strategic partner for the development of pharmaceutical production in Africa.
Reference Link
http://www.unaids.org/en/resources/presscentre/featurestories/2012/may/20120504india/
Regards
Dr Rajshree D. Katke.
M D (Obst & Gyanec), FIGOG
Medical Supertendent & Unit Head,
CAMA & ALBLESS Hospital, MUMBAI - 01
Clear Cell Carcinoma of the Uterine Cervix: A Case Series of Five Patients
Link
http://www.casereports.in/articles/3/2/Clear-Cell-Carcinoma-of-the-Uterine-Cervix-A-Case-Series-of-Five-Patients.html
http://www.casereports.in/articles/3/2/Clear-Cell-Carcinoma-of-the-Uterine-Cervix-A-Case-Series-of-Five-Patients.html
Dilip Sandipan Nikam, Rajshree Dayanand Katke
From
the Department of Radiotherapy & Oncology1, Department of
Obstetrics & Gynecology2; Cama & Albless Hospital, Grant
Government Medical College & Sir J. J. Group of Hospitals, Mumbai,
Maharashtra, India.
|
||||||||
|
||||||||
|
||||||||
|
||||||||
Introduction:
Cervical
cancer is the commonest cancer in Indian women where it is second most
common cancer and the fifth most common cause of cancer deaths in women [1,2]. Approximately 80% of cervical cancers occur in developing countries [3].
Clear cell carcinoma of the cervix (CCCC) is a rare subset of
adenocarcinomas that constitutes 10–20% of all the cervical cancer [4].
The diagnosis of the tumor is by histology. Histologically the tumor
cells have distinct clear, empty appearing cytoplasm and enlarged,
hyper-chromatic nuclei, which project into the apical cytoplasm, the so
called hobnail appearance. The clear cytoplasm is attributed to the
accumulation of abundant glycogen similar in appearance to that seen in
secretory endometrial cells. The cells grow predominantly in
tubulocystic, papillary or solid pattern. The most favorable outcome is
associated with the tubulocystic pattern, followed by the papillary and
solid patterns.In early 1970s, studies showed without any in-utero
exposure to diethylstilbestrol (DES), CCCC are rare and generally
post-menopausal [5,6].
Radical surgery for localized disease with adjuvant chemo-radiation in
patients with high-risk tumor characteristics is the current
recommendations for management of adenocarcinoma of the cervix [7,8].
In our case series study, we have evaluated 5 cases of CCCC with the
objectives of evaluating the treatment options and their clinical
outcome.
Case Series:
This
is retrospective analysis of treatment outcomes and response pattern in
patients with primary clear cell carcinoma of the cervix presenting at
the department of radiotherapy and oncology from January 2004 till
December 2010. Total five patients with primary clear cell carcinoma of
the cervix were registered.
The
average age of females in the study was 49 years ranging from 26 to 66
years, belonging to either middle or lower socio-economic strata with at
least one child. None of them had a family history of cancer or history
of DES exposure. The most common presenting symptom was bleeding per
vagina. Three of patients were IIB-FIGO stage, one IIA-FIGO stage and
one IB-FIGO stage. Two of the patients (IB,IIA) underwent Wertheim’s
hysterectomy, pathologic examination showed bilateral parametrium
involvement in one patients and the right parametrium involvement in
other patient. Two postoperative patients received adjuvant radiotherapy
while three patients received radical concurrent chemo-radiotherapy
along with weekly cisplatin. Out of three, two patients received five
courses of chemotherapy with cisplatin at 40 mg/m2. All
patients were added with intra-cavitary brachytherapy. On a follow up of
5 years, one patient who showed progressive disease died after 27
months, other patient defaulted follow up and the remaining three
patients had no relapse or metastasis and are on routine follow up. The
median follow-up was 44.5 months ranging from 27 months to 65 months.
Case 1:
66 year old post-menopausal women with no other significant medical or
family history presented with the complaints of bleeding and discharge
per vagina. Per-vaginal examination showed proliferative growth at
cervix measuring around 4 cm involving all fornixes, bilateral
parametrium were involved medially but not up to lateral pelvic wall and
rectal mucosa was free. CT/USG of abdomen showed a mass of size 3.8x3.3
cm at cervix with thickened endometrium and bilateral parametrial
involvement. Clinically it appeared to be of FIGO Stage II-B. The biopsy
of cervix confirmed the diagnosis of clear cell carcinoma of cervix.
The patient was treated with radiotherapy 50 Gy in 25 fractions and 2
doses ICRT in 50 days and 5 cycles of concurrent injection of cisplatin
at the dose of 40mg/m2. Follow up after 3 months showed progressive disease and the patient succumbed to death 27 months after the start of therapy.
Case 2:
A 50 year old post-menopausal woman presented with the complaints of
bleeding per vagina and a past history of tuberculosis with allergy to
sulfa drugs. No significant family history was noted. Per-vaginal
examination showed proliferative growth at cervix measuring around 4 cm
involving right fornix, right parametrium involved medially but not up
to lateral pelvic wall, free left parametrium and rectal mucosa. CT/USG
report showed 4x4 cm mass at cervix with right parametrial involvement.
Clinically it appeared to be of FIGO Stage II-B. The biopsy of cervix
confirmed the diagnosis of poorly differentiated carcinoma with clear
cell histology. The patient was treated with radical concurrent
chemo-radiotherapy 50 Gy in 25 fractions and 2 doses of ICRT in 59 days
and 5 cycles of injection cisplatin at the dose of 40 mg/m2. The patient showed clinically controlled disease on follow-up visits over 29 months.
Case 3:
A 43 year old pre-menopausal woman with history of diabetes mellitus
presented with leucovaria. Per-vaginal examination showed proliferative
growth at cervix measuring around 6 cm hanging into vagina, free
bilateral parametrium and rectal mucosa. CT/USG showed a mass measuring
4.3x5.4x5.2 cm. Clinically it appeared to be FIGO Stage IB2. Based on
the biopsy reports of the uterine cervix, it was diagnosed as
adeno-squamous tumor with 10% clear cell carcinoma of the cervix. The
patient underwent Wertheim’s hysterectomy for the same, histopathology
was reported as 7x7x1.5 cm mass infiltrating more than half thickness of
cervical stroma along with free bilateral parametrium, vaginal margins
and four pelvic lymph nodes [Fig.1]. She received radiotherapy of 50 Gy
in 25 fractions and 2 fractions of CVS brachytherapy in 47 days. The
patient was doing well following a five year follow-up.
Case 4:
A 26 year old pre-menopausal woman presented with bleeding per vagina.
Per-vaginal examination showed proliferative growth at cervix measuring
around 6 cm hanging into vagina, bilateral parametrium were involved
medially but not up to lateral pelvic wall and normal rectal mucosa.
CT/USG report showed 5.9×5 cm mass at cervix. Clinically it appears to
be FIGO Stage II-B. The biopsy of the uterine cervix confirmed the
diagnosis of clear cell carcinoma. The patient was treated with radical
concurrent chemo- radiotherapy 50 Gy in 25 fractions and 2 doses of ICRT
in 48 days and 5 cycles of injection cisplatin at the dose of 40 mg/m2. The follow up details of the patient is not available, as the patient defaulted.
Case 5:
A 60 year old post-menopausal woman with history of diabetes mellitus
and hemiplegia presented with bleeding per vagina. She also had history
of tobacco usage. Per-vaginal examination showed proliferative growth at
cervix measuring around 4 cm involving anterior fornix, bilateral
parametrium are free, rectal mucosa is normal. A mass of 4.5×3.5×2.5 cm
was noted on CT/USG. Clinically it appears to be FIGO Stage II-A. A
biopsy of the uterine cervix confirmed clear cell carcinoma. The patient
underwent Wertheim’s hysterectomy for the same [Fig.2], histopathology
were reported as 4.5x3.5x1.5 cm mass infiltrating more than half
thickness of cervical stroma. She received radiotherapy of 50 Gy in 25
fractions and 2 fractions of CVS brachytherapy in50 days. The patient
was doing well without clinical evidence of any disease, on a follow-up
visit after 5 years and 5 months.
| ||||||||
Discussion:
Although
most cervical carcinomas are squamous, a significant number are
adenocarcinomas. Adenocarcinomas are histologically categorized into
mucinous, endometrioid, clear cell, serous and mesonephric subtypes [1].
CCCC were a rare type of adenocarcinomas that affected the older women
before the DES era and in the DES era, its incidence increased in the
adolescent and young women; whose mothers were exposed to DES during
pregnancy. Following the ban on DES, non DES associated CCCC are
frequent. The median age of patients affected by this disease is 53
years and mean age of the patients in this series is 49 years. The
common symptom is generally irregular vaginal bleeding and the majority
of patients (80%) in the series presented with this symptom. The tumor
growth is endophytic and tend to show deep infiltration of the cervix
and also extend to the uterine corpus more often than other cervical
carcinomas [9].
It is histologically characterized by a mixture of clear and hobnail
shaped tumor cells arranged in solid masses and papillary tubule [1].
Early-stage CCCCs have a favourable prognosis and retrospective review
has shown that patients with early stage disease are amenable to surgery
and have a good overall survival. This review also discussed that CCCC
patients with bulky tumor, more than half stromal infiltration, positive
lymph nodes are at higher risk of recurrence and would appear to
benefit from chemo-radiation [8,9].
The prognosis of patients with early stage CCCC treated surgically and
noted to be free of lymphatic dissemination is excellent irrespective of
the use of adjuvant therapy. Traditional risk factors (positive lymph
nodes, positive surgical margins, parametrial involvement, tumor
diameter N4 cm, lymph vascular space involvement, and N1/3 cervical
stromal involvement) as indications for chemo-radiation should be
applied to patients with early stage CCCC. Similarly in our series, two
patients had operable disease hence underwent surgery. In view of high
risk for recurrence they received adjuvant radiotherapy; both these
patients are on regular follow up more than 5 years.
FIGO
stage IIB to IIIB, platinum based chemo-radiation improves the local
control and overall survival and is the mainstay of treatment. In our
series, three patients were stage IIB where two underwent concurrent
chemo-radiotherapy; among them one patient progressed and died
eventually after 27 months of treatment while other is having controlled
disease till date.
Small
observation studies have shown that surgery combined with chemotherapy
with carboplatin and 5-FU or paclitaxel may lead to relatively perfect
short-term therapeutic effect [10]. In our series, the chemotherapeutic agent used was cisplatin which showed good response in one of the patient.
Conclusion:
Post
Diethylstilbetrol era, primary clear cell carcinoma of uterine cervix
is a rare disease where patients with low risk early stage CCCC may be
managed with radical surgery alone, with or without the need for
adjuvant chemotherapy or radiation. Advanced stage CCCC should be
treated with a combination of platinum based chemo-radiotherapy [8].
References:
- Armstrong EP. “Prophylaxis of Cervical Cancer and Related Cervical Disease: A Review of the Cost-Effectiveness of Vaccination Against Oncogenic HPV Types”. Journal of Managed Care Pharmacy. 2010;16(3):217–230.
- World Health Organization February. 2006; “Fact sheet No. 297: Cancer”. Retrieved 2007-12-01.
- Kent, A. “HPV Vaccination and Testing”. Reviews in Obstetrics and Gynecology. 2010;3(1):33–34.
- Tamini HK, Figge DC. Adenocarcinoma of the uterine cervix. Gynecol Oncol.1982;13:335-338.
- Herbst AL, Ulfelder H, Poskanzer DC. Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med. 1971;284(15):878–881.
- Errarhay S, Mamouni N, Mahmoud S, El fatemi H, Saadi H, Mesbahi O, et al. Primary Malignant Melanoma of the Female Genital Tract: Unusual Localization. Journal of Case Reports. 2013;3(1):169-175.
- Chaudhari T. Primary clear cell adenocarcinoma of the uterine cervix in a young woman not associated with diethylstilbestrol: A case report and review of literature. Available at http://www.ccij-online.org/text.asp 2012/1/4/239/106278. Accessed on 12 September 2013.
- M. Bijoy Thomas, Jason D Wright, Aliza L Leiser, Dennis S Chi, David G Mutch, Karl C Podratz et al. Clear cell carcinoma of the cervix: A multi-institutional review in the post-DES era; Gynecologic Oncology. 2008;109:335–339.
- T. Hiromura, O Tanaka, T Nishioka, M Satoh, M Tomita. Clear cell adenocarcinoma of the uterine cervix arising from a background of cervical endometriosis; The British Journal of Radiology. 2009;82:e20–e22.
- Tan YT, Zhang X, Lin ZQ, Chen Q, Wang LJ, Zhang BZ. Primary clear cell carcinoma of the cervix: report of five cases and review of the literature. Zhonghua Fu Chan Ke Za Zhi. 2008;43(2):120-123.
Subscribe to:
Posts (Atom)